Angela Brivio
Consultant Knee Surgeon,
MD FRCS
Hello, Welcome to the website.
I’m Angela Brivio and my goal is to get the best results for my Knee patients to let them achieve their better Life quality and activities.
I’m keen on knee surgery: from arthroscopies and ligament reconstruction in the young athlete, till arthroplasties and revision knee surgery in the more mature patient.
I’ve attended several knee surgery centers in Italy, France and England.
I’m based at Città Studi Hospital in the center of Milan, working and teaching as a Knee expert, but regularly visit London to operate and work as a consultant knee surgeon at King Edward VII Hospital.
I regularly take part in national and international congresses to get up-to-date.
I’ve done scientific research and I carry on studying knee arthroplasty and prosthetic design, to whom I dedicated my last years.
I’m firmly convinced that every patient needs his own path through the operation and rehabilitation and my aim is to follow him throughout his whole way from diagnosis till rehab after surgery. With this target I developed with English colleagues and “My Recovery” team, un app for every knee surgery, tailored for each patient.
If you see something that interest you here, get in touch directly.
About me
My experience
I studied Medicine and Surgery at the University of Milan, and partly in Strasbourg, where I discovered my passion for Orthopaedics and Traumatology.
I specialised at the University of Milan, with a thesis on elbow fractures in children that I later published.
I took my study to a three-year world congress (SICOT/SIROT) in Hong Kong in 2008.
I dedicated the first years of my career to paediatric orthopaedics and traumatology as my interest in the knee grew.
Thus, I started attending courses and congresses, as well as visiting the operating theatres of distinguished knee surgery colleagues in Italy and abroad.
I was in Berlin in 2015 at a meeting on revision knee surgery, in Knokke (Belgium) in 2016 at the “PKM”, a European congress on monocompartmental (partial) knee replacements, in Oxford in 2017 at an education course on partial knee replacements, in Valencia, in Bruges …
I believe it is fundamental in my work to meet, compare and collaborate with colleagues.
I worked in 2017-2018 in the Department of Prosthetic Surgery at the Galeazzi (Milan) with Prof. Sergio Romagnoli, a luminary in knee prosthetics and in particular in monocompartmental and bimonus prostheses.
I have recently developed a personal smartphone application in order to better accompany my patients step by step through the surgery and rehabilitation process.
In April 2021 I joined the GMC (General Medical Council), the UK Medical Council, and started working with Professor Barrett as a consultant for Knee Surgery.
In 2022, I joined the European Knee Society as a Junior Member and became a Royal College of Surgeons (FRCS) in July 2022.
In June 2023 I became a Tutor in Knee Course on “Advanced Course on Unicompartmental Knee Replacement” at ICLO Teaching and Research Center in Verona
In January 2024 I became and Active Member Of the European knee Ho attualmente il ruolo di Academic Visitor all’Imperial College di Londra.
I was invited to join the consultant staff at King Edward VIIth’s Hospital as a Consultant Knee Surgeon working alongside along Prof. David Barrett and Prof. Justin Cobb. I practiced at KEVII Hospital till July 2024.
I have been a member of the regular review board for knee surgery at King Edward VII’s Hospital, where all cases are discussed and evaluated.
I have an active interest in research and academic knee surgery as well as the treatment of complex knee conditions. I am actually an Academic Visitor at Imperial College London at the Department of Mechanical Engineering where I am developing some projects about knee prosthetic design.
The knee remains the focus of my work.
If you find something on the site that intrigues you and you would like to get to know me, please do not hesitate to get in touch.
My Team
I work with Dr. Nicolò Castelnuovo at ICCS – Istituto Clinico Città Studi – in Milan. With Nicolò I share a passion for knee surgery, operating with him on this joint at 360 degrees. In addition to traditional surgery, we are developing Robotic Surgery, conducting scientific studies and collaborating with leading companies in the field of knee prosthetics.
I also work at the “I Cedri” Clinic in Fara Novarese (NO) together with Dr. Castelnuovo and Dr. Giacomo Zanon, with whom I carry out Sports Medicine surgeries.
Interests
An activity that I have loved doing for a long time as a hobby is teaching in primary and secondary schools.
I really enjoy teaching anatomy to children and young people, I prepare interactive lessons and I love lively participation from the students, who are thus involved in the learning process in a dynamic and fun way.
To see my curriculum vitae in detail click here.
Procedures
Arthroscopy has become vastly popular as a means of examining and treating conditions affecting the joints.
Most arthroscopic procedures are carried out upon the knee joint, which because of its complexity and design is the most commonly injured large joint in the body. For instance, over two million arthroscopies are carried out per year in the United States.
The procedure is safe and reliable in expert hands and represents what most people would know as minimal access surgery or keyhole surgery.
The advantages to the patient include extremely small incisions and ease of mobilisation after the procedure.
This renders most arthroscopic procedures day case activities with rapid return to full function and work status.
PROCEDURES
A vast number of operative procedures are possible during arthroscopy in addition to inspection of all the joint surfaces and the two menisci in the joint. Powered arthroscopic instruments and micro tools are available in specialized knee units which allow complex procedures to be carried out down the arthroscope.
The majority of the operations down the arthroscope are performed on the meniscal cartilages within the joint. Additionally surgery to the anterior cruciate ligament, which is situated in the central part of the knee joint and repair or smoothing down of articular cartilage (which lines the surfaces of the knee) is also possible as well as complimenting microfracture and cartilage repair techniques.
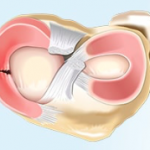
MENISCAL SURGERY
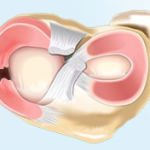
The menisci (cartilages) are the structures on which most of the work is carried out during an arthroscopy. Due to the design of the knee, the menisci are crucial to its function both in bending and flexing and in twisting or pivoting. The menisci act as a washer or shock absorber within the joint allowing smooth movement of the femur upon the tibia. The menisci also aids distribution of the lubricant fluid within the knee and thus aid the articulation of the joint and the friction free movement of the bones.
The menisci may be injured by sudden trauma, such as a sporting accident, or a twisting injury. Alternatively the menisci may tear as a result of minor repetitive injury associated with active movement or prolonged sporting activity. Once the menisci are torn, the damaged edge of the meniscus becomes obstructed to the normal movement of the joint and pain results, particularly worsened by deep knee bends or twisting movements. As well as pain, some long term damage can occur as a result of the torn cartilage damaging the bearing surface of the joint.
Meniscal surgery to a damaged articular cartilage is directed at removing the area which is torn, whilst leaving the vast majority of undamaged meniscus intact. Previous studies have shown that removal of the entire meniscus results almost certainly in osteoarthritic degeneration of the knee as the lubricant and washer facilities of the cartilage are removed and the bone of the femur begins to grate on the bone of the tibia.
Every effort is therefore made to leave as much good meniscal tissue as possible. Should the meniscal tear occupy less than 30% of the surface area, there are few long term symptoms, as the remaining 70% of the meniscus will cope adequately with the weightbearing duties of the knee.
Meniscal damage that involves more than 30% of the surface area of the structure will be repaired to maintain its washout and lubricant function. Fortunately the majority of meniscal tears that do occur are less than the critical 30%.
ARTICULAR CARTILAGE SURGERY
Articular cartilage forms a vital function within the knee joint, coating the bearing surfaces of the femur, the tibia and the under surface of the patella or knee cap. The special qualities of this articular cartilage lining the joint allow the bones to move together with a minimum of friction and wear. It has been observed that the friction between the femur and tibia is actually less than that of two smooth blocks of ice sliding on each other.
However the smooth lining of the joint may be damaged by injury leading to painful symptoms as parts of the underlining bone are exposed, giving rise to grating and crunching symptoms along with pain and aching.
Once damaged, articular cartilage does not regenerate and there is the possibility that damage to the articular cartilage can extend.
Arthroscopic surgery is aimed at containing and smoothing these areas and promoting the growth of repair tissue.
This repair tissue is basically scar tissue but in many cases this can alleviate some of the discomfort and prevent further damage to existing articular tissue.
Other specialist techniques such as microfracture and cartilage grafting may be necessary to restore some of the function of the joint.
ATTACHMENTS
PREAMBLE
Over the last 10 years advances in surgical technique and joint design have meant that knee joint replacement has become a reliable and rewarding procedure, relieving pain and in many cases improving range of movement of a diseased joint with great success. What follows is some information and data on the particular joint or replacement you may receive as well as some information concerning the operation, rehabilitation and recovery.
HISTORY
Arthritis of the knee joint has caused many problems for surgeons since the beginning of orthopaedics. It has been difficult to treat successfully and until relatively recently knee surgery was regarded as a fairly risky undertaking with often quite poor or disappointing results. Some years ago it was common practice to remove the knee joint entirely and substitute a simple metal hinge inside the bone to allow the patient to bend the knee. This often resulted in failure and unfortunately gave knee surgery a poor reputation and standing amongst the general public.
Radical redesign of the materials and joint inserted into the knee however has improved beyond all recognition the results from this operation and now 95% of people undergoing knee joint replacement may expect good to excellent results if the operation is performed by a specialist knee surgeon.
KNEE JOINT DESIGN
The more recent designs of knee joint concentrate on replacing the worn bearing surface of the knee and to keep all the other natural components of the joint such as the surrounding ligaments, soft tissues and knee cap. This allows minimal removal of the patient’s own tissues and just resurfaces the areas that are worn; as a result the knee is felt to move more naturally and results of these more modern prostheses are most satisfactory.
FEMUR
The femur is shaped to resemble the real bearing surface of the end of the thigh bone and is a complex design made of a type of stainless steel which is tolerated by the body’s own natural tissues. The tibia is resurfaced by a platform of metal on the top of which is situated a bearing surface made of plastic. This in many ways resembles the cartilages that are naturally in a normal knee joint.
The plastic is made of a specially designed high density polyethylene and allows the bearing surface of the femur to move upon it.
ATTACHMENTS
PREAMBLE
Significant advances in total knee resurfacing (TKR) have meant that this is a much more reliable and satisfactory operation than ten or fifteen years previously. The success of total knee resurfacing has allowed surgeons and engineers to develop the concept of partial knee resurfacing to deal with patients developing the early changes of osteo-arthritis in isolated areas of the knee. These patients have a very much higher activity profile than those with total knee arthritis.
INDICATIONS FOR PARTIAL KNEE JOINT RESURFACING
In an age of increasing patient activity and sporting interests through middle life, and with the development of more sophisticated ways of analysising knee joint deterioration, it has been possible to identify patients who are experiencing early wear in specific parts of their knee joint.In the past these patients might have been advised to give up their sport or reduce their activity until a time where the wear had spread throughout the whole of their joint and their mobility and activity decreased entirely. They then were offered a total knee joint replacement. Nowadays advancing design has made it possible to resurface these isolated parts rather than wait for the entire joint to deteriorate and the patient’s mobility to decrease. The object is to keep the patient mobile and active, whilst resurfacing only the damaged area of the joint in a much smaller and reduced operation. There are many advantages in undergoing a smaller procedure with more rapid rehabilitation and greater activity at an earlier stage following operation.
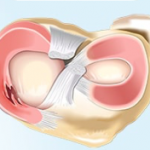
MEDIAL (INNER) KNEE JOINT WEAR
Approximately 80% of knee patients will begin to wear on the inner aspect of their joint, prior to the rest of the joint being involved. Patients present with pain on the inner aspect of the joint related to activity or movement which is easy to pinpoint and becomes more troublesome and tiresome related to activity, but then later even more minor activities cause discomfort and sleep may be disturbed.
The articular cartilage or lining cartilage of this aspect of the joint becomes worn down and the bone of the femur and tibia begin to grind together to cause pain and discomfort. At this early stage it is possible to resurface just the inner aspect of the femur and tibia with a very thin lining of a special medical grade of stainless steel which is implanted on top of the bony surfaces. To prevent the two metal surfaces grinding together a small plastic bearing is inserted on to the top of the tibial plate to allow easy articulation.
The advantages of this procedure is that none of the ligaments around the knee or indeed inside the knee are disturbed by this procedure which is simply a recoating or relining of the worn areas of the joint. This bearing replicates the role of the cartilage in the natural knee.
The prosthesis used for this resurfacing procedure is the SIGMA high performance resurfacing prosthesis (see Links section) made by DePuy, a Johnson & Johnson Company. This prosthesis has been recently developed purposefully for the more active patient and also has a number of features which allows it to be revised or added to as various other parts of the joint may wear out in the future in an active patient.
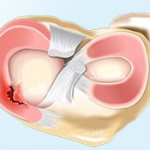
LATERAL (OUTER JOINT) RESURFACING
The mechanism of wear which causes eventually the bones to grind together on the outside aspect of the joint is very similar to that described for the medial or inner joint wear process. The minority of patients (20%) wear their knee initially on the outer aspect and this may reflect a degree of malangulation which may have been present since youth.
Nevertheless, the bone grinding on bone produces very similar pain and discomfort to that on the inner aspect of the joint and if the rest of the knee remains intact, lateral (outer joint) resurfacing is a very similar procedure to that of inner or more medial resurfacing.
Those looking for information in different sources and different websites may find that surgeons will state that resurfacing may only be performed on the medial or inner side and that lateral or outer resurfacing is not advised.
This does represent a historical standpoint and in the past outer joint resurfacing was discouraged as the results were disappointing.
There are some implants that are only designed for inner joint resurfacing such as the Oxford component. Redesign and more advanced techniques however have allowed a new concept which is equally implantable on the inner or outer aspect of the knee, this being the SIGMA high performance resurfacing prosthesis.
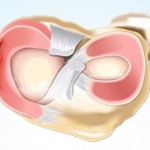
PATELLOFEMORAL (KNEECAP) RESURFACING
Isolated patellofemoral resurfacing is a procedure in which only the worn out and bare bone surface of the under surface of the kneecap or patella and the front surface of the femur (trochlear) are resurfaced with a metal prosthesis for the trochlear and a polyethylene or plastic surface cemented onto the patella. The attraction here of course is that if only the patella or kneecap is worn the patient may keep the rest of the natural or native knee without operation whilst a much more reduced procedure is performed to resurface the patellofemoral joint.
The procedure is much more minimal than that undertaken with total knee replacement and the patients are up and mobile often three times more quickly than with a larger procedure.
In the long term there is the possibility that further activity may cause wear and tear in the main joint of the knee but such is the patellofemoral joint employed, it is possible to resurface any extra areas of wear and tear when those occur rather than employing a total knee joint replacement at that time.
MULTI COMPARTMENTAL RESURFACING
Occasionally it is found that patients have worn in two of the three areas of the knee but because of their age and activity, total knee joint replacement is not desirable. In those isolated cases a very new and developing field of surgery is to resurface two out of three of these areas such as the patellofemoral and inner aspect of the knee or indeed the outer aspect of the knee and the patellofemoral joint, which allows the knee to keep its natural cruciate ligaments and the majority of the ligaments around the joint. This is a new and specialised procedure and may only be undertaken in patients who are particularly suitable for the operation.
The advantages however mirror those of partial resurfacing with more activity being possible in the post surgery period and much more rapid recovery.
ATTACHMENTS
PREAMBLE
The anterior cruciate ligament is a complex and vital central structure to the stability and function of the knee joint in both sports and the activities of daily living. Breakage of this ligament may lead to instability of the knee, preventing sports participation and pivoting movements. Long term instability with giving way of the joint has been associated with premature wear and tear changes or osteo-arthritic change in the joint.
Over the last 12 years, significant advances in the technique and surgery of the anterior cruciate has allowed effective reconstruction of this ligament with encouraging successful results in the hands of the specialist surgeons.
What follows is information on the anterior cruciate ligament, its structure and function and an overview of the surgery and important rehabilitation points for patients undergoing anterior cruciate ligament (ACL) reconstruction.
ANATOMY
The anterior cruciate ligament arises from the mid portion of the tibia at its upper surface and then passes diagonally backwards to the most rear aspect of the femur. Its fibres are orientated in a complex spiral fashion and the ligament itself receives an excellent blood and nerve supply from both the femur and tibia.
The nerve supply to the anterior cruciate ligament is important in allowing the co-ordination centres of the brain to plan and execute complex knee movements. These movements are vital in pivoting and twisting that occur in sports activities.
FUNCTION
The knee joint is capable of flexion and extension, rotation and a degree of gliding back and forth. During these complex compound movements the femur and tibia are held together by the anterior cruciate ligament, which is the most important or primary restraint to the knee under these conditions.
Other ligaments around the knee aid in stability, but they are of less or secondary importance to knee joint stability.
A loss of the anterior cruciate ligament therefore allows the femur to move in an unnatural and unrestrained way on the top of the tibia during movement. As a result under certain circumstances, the femur can slip off the top of the tibia and a partial knee dislocation or “giving way” results.
This has two sequelae: collapse of the knee and failure to function and secondarily, abnormal movement of the knee may cause further cartilage injury. This, in the long term, is associated with degenerative change or osteoarthritis in the knee at a later stage.
Reconstruction of a symptomatic knee therefore is aimed in the short term at restoring function and pivoting ability to the joint and in the long term by stabilisation of the knee, preventing any early wear and tear changes or subsequent cartilage damage.
RECONSTRUCTION
The anterior cruciate ligament breaks under tremendous stress. The ligament fails catastrophically and patients are sometimes aware of a “crack” as the ligament fails. Although surgeons in the past have attempted to repair the torn ligament, there is very good research evidence that simple suture of the ligament is not strong enough to restore normal function to the joint. A replacement structure must be used to take the place of the anterior cruciate ligament. Some years ago artificial fibres such as gortex and carbon fibre were used to reconstruct the anterior cruciate ligament, but all artificial fibres failed two years post surgery and these reconstructions were not successful.
Currently, other ligaments around the knee with the same strength as the original anterior cruciate ligament are employed as a ligament reconstruction. Use of the patient’s own ligaments as donor tissue is attractive because there is no fear of graft rejection nor any of the attendant problems of using artificial materials within the human body.
There are two donor tendons which can be used for anterior cruciate reconstruction. One third of the patellar tendon may be used as a donor ligament and published research indicates that over a long follow up period, this is a successful and safe ACL reconstruction. An alternative donor tissue are hamstring tendons which are harvested from the same knee on the inner aspect. These tendons are more suitable for certain types of patient and both procedures involve a small scar over the front part of the knee and currently there is no difference in published research regarding different donor tissues, they both seem to give identical long term results.
ATTACHMENTS
Contacts
Enjoy Sport Center
Via Michelangelo Buonarroti, 44A
20063 Cernusco sul Naviglio (MI)
Tel: +39 02.9241256 (int. 4)
Web: www.enjoysport.eu
StudioEFFE
Via dei Mille, 41
20851 Lissone (MB)
Tel: +39 333 906 2032
Web: https://www.instagram.com/fisioeffemed/
ICCS – Istituto Clinico Città Studi
Via Jommelli, 17
20131 Milano
Tel: +39 02.23932041
Web: www.ic-cittastudi.it